Decoding the 12 Lead EKG CPT Code: A Comprehensive Guide
The 12 lead EKG, or electrocardiogram, is a fundamental diagnostic tool in modern medicine. It provides a detailed snapshot of the heart’s electrical activity, aiding in the diagnosis of various cardiac conditions. Crucial to the billing and reimbursement process for this essential procedure is understanding the correct CPT (Current Procedural Terminology) code. This article delves into the intricacies of the 12 lead EKG CPT code, exploring its components, applications, and the nuances that healthcare professionals and billing specialists need to know. Proper utilization of the 12 lead EKG CPT code ensures accurate billing and facilitates the smooth operation of healthcare facilities. The information outlined below will help you navigate the complexities of the 12 lead EKG CPT code.
What is a 12 Lead EKG?
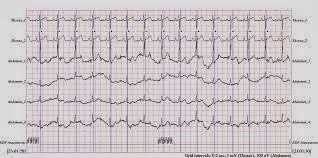
Before diving into the specifics of the CPT code, it’s important to understand what a 12 lead EKG entails. A 12 lead EKG uses ten electrodes placed on the patient’s limbs and chest to record the heart’s electrical activity from twelve different angles, or “leads.” This comprehensive view allows physicians to identify abnormalities like arrhythmias, ischemia, and heart attacks. The 12 leads provide a detailed representation of the heart’s electrical function, making it an indispensable tool in cardiology.
Understanding CPT Codes
CPT codes are standardized numerical codes developed and maintained by the American Medical Association (AMA). These codes are used to report medical, surgical, and diagnostic procedures and services to insurance companies and other payers. Accurate CPT coding is essential for appropriate reimbursement and compliance with healthcare regulations. The 12 lead EKG CPT code is a specific example of how these codes are used in practice.
The Specific 12 Lead EKG CPT Code
The primary CPT code for a standard 12 lead EKG is 93000. This code encompasses the routine performance, interpretation, and report of a 12 lead electrocardiogram. It is important to note that this code typically includes all three components: recording the EKG, interpreting the results, and generating a written report. Using the correct 12 lead EKG CPT code is crucial for proper billing.
Components of Code 93000
- Recording: This involves the placement of electrodes and the actual recording of the heart’s electrical activity.
- Interpretation: A physician or qualified healthcare professional must review the EKG tracing and interpret the findings.
- Report: A written report summarizing the interpretation and any significant findings must be generated.
Variations and Additional Codes
While 93000 is the primary code, there are situations where additional or alternative codes may be necessary. These variations often depend on the specific circumstances of the EKG administration and interpretation.
93005: Electrocardiogram; Tracing Only, Without Interpretation and Report
This code is used when the EKG tracing is performed, but the interpretation and report are done by a different provider. For example, a technician might perform the EKG, and a cardiologist at a remote location interprets the results. In this scenario, the technician’s facility would bill using code 93005, while the cardiologist would use a different code for the interpretation.
93010: Electrocardiogram; Interpretation and Report Only
Code 93010 is used when a physician interprets and reports on an EKG tracing that was performed elsewhere. This is common in telemedicine or when a primary care physician refers an EKG tracing to a cardiologist for expert interpretation. It is essential to coordinate billing to avoid duplicate charges.
93042: Rhythm ECG, 1-3 Leads; With Interpretation and Report
This code is used for a rhythm EKG, which typically involves fewer leads (1-3) and focuses on monitoring the heart’s rhythm over a period of time. This differs significantly from the 12 lead EKG, which provides a comprehensive view of the heart’s electrical activity. Ensure accurate coding by distinguishing between a rhythm EKG and a full 12 lead EKG.
Modifiers and Their Impact
Modifiers are two-digit codes added to CPT codes to provide additional information about the service or procedure performed. They can indicate that a service was altered, performed by more than one provider, or involved special circumstances. Understanding and using modifiers correctly is crucial for accurate billing and avoiding claim denials.
Modifier 26: Professional Component
Modifier 26 is used when a physician provides only the professional component of a service, such as the interpretation and report of an EKG. This is often used in conjunction with code 93005 when the interpretation is performed by a different provider than the one who performed the tracing. The 12 lead EKG CPT code with modifier 26 indicates the physician’s professional service.
Modifier TC: Technical Component
Modifier TC is used to indicate the technical component of a service, such as the equipment and personnel costs associated with performing the EKG tracing. This modifier is often used in conjunction with code 93010 when the facility provides the technical component, but the interpretation is performed by an outside physician.
Common Billing Errors and How to Avoid Them
Billing errors can lead to claim denials, delays in reimbursement, and potential compliance issues. Understanding common errors associated with the 12 lead EKG CPT code can help healthcare providers and billing staff avoid these pitfalls.
Unbundling
Unbundling occurs when a single procedure is broken down into its component parts and billed separately. For example, billing separately for the electrode placement, recording, interpretation, and report when all are included in code 93000 is considered unbundling. This practice is generally not allowed and can result in claim denials.
Duplicate Billing
Duplicate billing occurs when the same service is billed more than once for the same patient on the same date of service. This can happen if multiple providers are involved in the EKG process and are not coordinating their billing. Careful coordination and accurate documentation are essential to prevent duplicate billing.
Incorrect Modifier Usage
Using the wrong modifier or failing to use a modifier when necessary can lead to claim denials. For example, using modifier 26 when the physician performed both the tracing and interpretation is incorrect. Always verify the specific circumstances of the service and select the appropriate modifier accordingly.
Documentation Requirements
Accurate and complete documentation is essential for supporting the use of the 12 lead EKG CPT code. The medical record should clearly document the following:
- The date and time of the EKG.
- The reason for performing the EKG (e.g., chest pain, shortness of breath).
- A detailed description of the findings and interpretation.
- The name and credentials of the healthcare professional who performed the interpretation.
- A copy of the EKG tracing.
Proper documentation not only supports billing but also ensures continuity of care and facilitates accurate medical decision-making.
Staying Up-to-Date with Coding Changes
CPT codes are updated annually by the AMA, and it is crucial for healthcare providers and billing staff to stay informed of these changes. Changes can include new codes, revised codes, and deleted codes. Subscribing to coding newsletters, attending coding seminars, and consulting with coding experts are effective ways to stay up-to-date.
The Importance of Accuracy in Billing
Accurate billing is essential for the financial health of healthcare practices and for maintaining compliance with healthcare regulations. Using the correct 12 lead EKG CPT code, understanding modifiers, and avoiding common billing errors are all critical components of accurate billing. By investing in proper training and resources, healthcare providers can ensure that they are billing correctly and receiving appropriate reimbursement for their services.
Impact of Telehealth on EKG Coding
The rise of telehealth has introduced new considerations for EKG coding. When EKGs are performed remotely, it is crucial to accurately document the roles of each provider involved. For example, if a technician at a remote location performs the EKG and transmits the tracing to a cardiologist for interpretation, the appropriate codes and modifiers must be used to reflect this arrangement. Telehealth EKG services often utilize the 12 lead EKG CPT code in conjunction with telehealth-specific modifiers, when applicable. [See also: Telehealth Billing Guidelines]
Future Trends in EKG Technology and Coding
As technology advances, EKGs are becoming more sophisticated, with features like continuous monitoring and advanced analysis algorithms. These advancements may eventually lead to changes in CPT coding to reflect the increased complexity of these services. Staying informed about these trends is essential for healthcare providers and billing staff to ensure they are prepared for future coding changes. The evolution of EKG technology will likely impact how the 12 lead EKG CPT code is utilized and potentially updated. [See also: Advances in Cardiac Monitoring]
Conclusion
Understanding the 12 lead EKG CPT code and its nuances is essential for accurate billing and compliance in healthcare. By mastering the components of the code, recognizing variations and modifiers, avoiding common billing errors, and staying up-to-date with coding changes, healthcare providers and billing staff can ensure they are receiving appropriate reimbursement for their services. Accurate coding not only supports the financial health of healthcare practices but also contributes to the overall efficiency and effectiveness of the healthcare system. Proper utilization of the 12 lead EKG CPT code is a fundamental aspect of healthcare revenue cycle management, leading to improved financial outcomes and better patient care.
